Once the stage of the investigations is completed, the gynecologist will welcome the couple during a consultation to discuss the appropriate treatment and the options available. The choice of treatment will obviously be based on the results of the examinations obtained and it is important at this level that the partners can position themselves in relation to their questions and hesitations. The proposed techniques will focus on 3 levels of assisted reproduction:
1. Ovarian stimulation for targeted sexual intercourse and inseminations
According to the results of the etiological assessment, in the event of an ovulation-related disorder and the absence of other causes in the couple, the gynecologist may first choose to address this problem by ovarian stimulation. This hormonal treatment concerns women and essentially aims to promote the simultaneous development of several follicles (stimulation of follicular growth) and to prevent spontaneous ovulation.
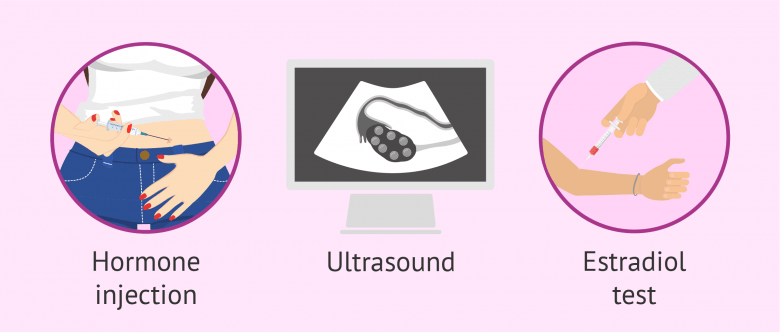
This treatment can be carried out either by oral medication or by daily injections depending on the active ingredient. These preparations may contain hormones with functions similar to that produced by the body FSH / LH.
During treatment, monitoring of the reaction of the ovaries to stimulation will be necessary, using ultrasound and blood tests. According to the information obtained from the monitoring, the attending physician will indicate to the couple the most fertile period of the female cycle and the most favorable to target sexual intercourse for pregnancy. Directed intercourse may or may not be associated with ovarian stimulation.
2. Artificial insemination (AI)
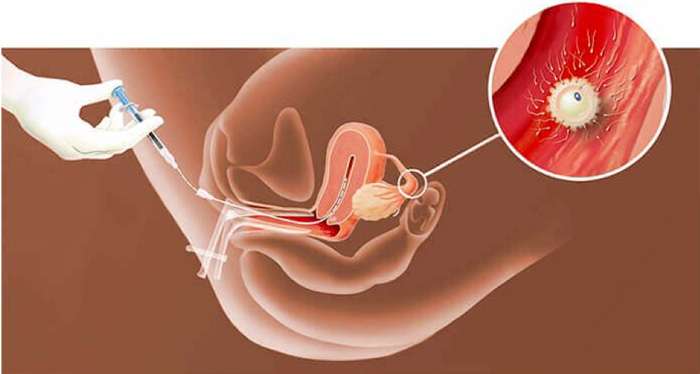
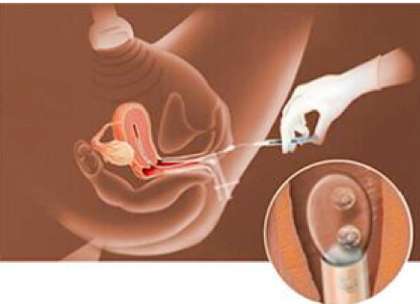
Partner’s semen artificial insemination (AI), also called intrauterine insemination (IUI), is a simple, painless technique that involves getting as many sperm as possible to the fertilization site. Sperm, fresh or frozen, is pre-prepared in the laboratory before being injected into the uterine cavity using a catheter. This procedure is quick and is performed in the examination room. Usually there are no activity restrictions after an AI. A blood pregnancy test is taken after fourteen days.
In practice :
-
- It is recommended that you drink water and come with a full bladder before the procedure to facilitate insemination.
- You will be notified 1 or 2 days before the procedure, depending on the spontaneous LH surge or ovarian stimulation (monitoring)
- In the case of insemination of fresh semen, the partner must arrive at least 2 hours before the procedure. The collection of the semen sample must be carried out in the laboratory.
- The procedure is performed in a gynecological position in the examination room.
3. In Vitro Fertilization (IVF)
In Vitro Fertilization, or IVF, is a laboratory technique where the oocyte and sperm meet in the laboratory, outside the woman’s body. It is thus necessary to have the oocytes of Madame and the sperm of the partner in the laboratory. For Monsieur, the sample collection is similar to the AI. On the other hand, for Madam, the procedure is more complex than that by AI: ovarian stimulation is more intense and the oocytes must be collected during a surgical procedure: the oocyte puncture.

This technique is usually performed after a series of unsuccessful AI procedures, for reasons of old age (over 35 years) or other cause of infertility.
Concerning fertilization in the laboratory, two techniques are available:
Classic IVF
The technique consists of bringing a large number of spermatozoa, prepared beforehand, into contact with the collected oocytes. The gametes are placed in a culture dish before being incubated. Fertilization during conventional IVF occurs naturally and spontaneously, provided the sperm is healthy or moderately damaged.
ICSI : Intracytoplasmic Sperm Injection
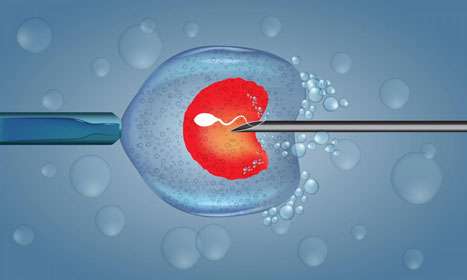
In case of conventional IVF presents a risk of failure due to insufficient sperm quality, the doctor may opt for the ICSI procedure. This technique involves choosing and aspirating a good quality sperm and introducing it directly into the egg, all under a specially equipped microscope. ICSI is being prescribed more and more compared to conventional IVF because of the significantly higher success rates achieved.
OTHER TECHNIQUES ASSOCIATED WITH IVF TREATMENT

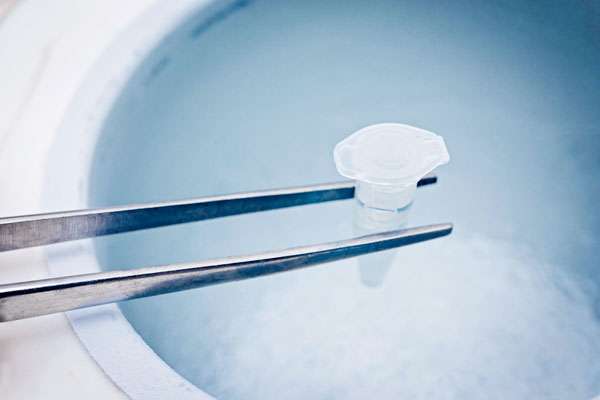
Freezing embryos: cryopreservation
Cryopreservation allows to preserve supernumerary embryos that have not been transferred during ongoing IVF treatment.
This technique is called vitrification where, if the quality and appearance of the embryo allow it, the fertilized oocytes are frozen and stored at a temperature of -196 degrees centigrade.
The goal of this technique is to have the possibility of performing other embryo transfers in the future, without having to redo the steps of ovarian stimulation and oocyte puncture. This process therefore allows you to transfer frozen embryos once again in the case of the absence of pregnancy or in the case of a desire for another child after a successful pregnancy.
Note that embryo freezing requires the consent of the couple prior to IVF treatment. If you do not want to freeze, you must notify the laboratory before starting the IVF procedure.
Embryo transfer
Embryo transfer is a simple and painless medical procedure that involves selecting 1 to 2 good quality embryos to transfer inside the uterus, using a thin catheter and under ultrasound control. Similar to the procedure by IUI, the transfer is performed in a gynecological position in a transfer room dedicated for this purpose. It is recommended that the patient arrive with a full bladder on the day of transfer to facilitate the procedure.
This procedure usually takes place after a short period of embryo culture, 3 to 5 days, in the case of a fresh embryo transfer. The transfer procedure can also be performed for embryos that have been frozen beforehand.
After the transfer, an appointment will be arranged after one to two weeks in order to take a blood test and check whether a pregnancy has started. Your gynecologist will continue to follow you whether or not you are pregnant and, if so, try to explain the reasons for the failure.
Preservation of fertility: sperm / oocyte freezing
Thanks to freezing and cryopreservation techniques, you have the opportunity today and at the Avicenne ART center to preserve your fertility by simply requesting our services. Freezing your eggs or sperm will allow you to postpone any childbearing.
Our entire team is at your disposal to discuss it with you and guide you in your choices.

Fertility surgery
Certain female or male pathologies can be the cause of infertility in the couple where a surgical act would represent an alternative to IVF and allow to improve the reproductive function.
In some cases, surgery may be an alternative or even a mandatory step before fertility treatments. The techniques most often used in fertility surgery are endoscopic such as hysteroscopy or laparoscopy.
In practice, these operations are performed under general anesthesia and on an outpatient basis (a few hours). In general, the patient can return home the same day as the operation. In more complex cases such as deep endometriosis, hospitalization of 24 to 48 hours may be necessary.
The laparoscopic surgical approach is offered in certain cases of infertility such as:
-
- Detection of the presence of lesions: endometriosis, fibroids, cyst. The treatment of these pathologies is carried out at the same time
- Treatment of polycystic ovary syndrome (PCOS) with a technique called “Ovarian Drilling”
- Tubal repermeabilization after voluntary sterilization
Some surgeries in the field of urology-andrology for Monsieur include: testicular biopsy, cystoscopy, vasectomy or Peyronie’s disease.



